MODEL THE COMPLEXITY
Step by step
Helping stroke patients regain mobility
By Kate Foster
“It just an average day,” Anna recalls. “The usual ups and downs at work, a gym class, then a glass of wine with a friend on the way home, nothing extraordinary.” But it was just as Anna had curled up on the couch to scroll through her social media feeds and catch up on her messages that she realized that the day had been anything but ordinary for family friend, Peter. “There it was: a group chat message saying that Peter had suffered a stroke that morning and was in hospital. I automatically thought of the last time I saw him at a get-together, just a week ago; he was tending to the barbecue and telling us about his upcoming ski trip. I was just shocked. It was hard to imagine him as a stroke patient.”
Anna’s reaction highlights the intrinsic nature of such medical events. They are so sudden, so quick, so seemingly indiscriminate. Strokes, or cerebrovascular accidents (to use medical terminology), are life-changing moments that strike the patient down, often out of the blue. Recovery is a long process. For many sufferers, this involves relearning even the most taken-for-granted actions, like walking and talking.
A growing challenge
It’s a story that, across the world, is all too common. The World Health Organization (WHO) estimates that 15 million people per year suffer a stroke[1]. Often, a stroke results in brain damage due to the sudden reduction in blood flow to the brain cells. It is estimated that, after three months, 20 percent of people who lost mobility as a result of a stroke remain wheelchair bound, while approximately seventy percent of sufferers walk at reduced velocity[2]. In many cases, patients undergo a lengthy and gruelling period of rehabilitation in order to re-establish the muscle strength, balance and range of mobility that they lost.
The reality is that stroke rates are increasing. According to a 2020 research report[3], the number of people living with stroke is estimated to increase by 27 percent between 2017 and 2047 in the European Union, mainly because of population ageing and improved survival rates. And given the prevalence of neurological and physiological damage following a stroke, the need for effective rehabilitation methods is acute.
But for stroke patients like Anna’s friend Peter, there is some positive news. Modern rehabilitation methods are embracing not only proven repetitive, task-specific approaches, but also cutting-edge technologies that are enabling people to walk again and re-establish their independence and quality of life more quickly. Much research is being done in this area and the technological advancements that are emerging in this space are encouraging. One such field is that of robotic exoskeletons, wearable mechanized devices that assist gait rehabilitation by amplifying and assisting natural motion.
Explainer: What happens during cerebrovascular accidents?
Put simply, a stroke is an attack on the brain; when the blood supply to part of the brain is cut off, it causes damage to brain cells and results in impaired neurological and physiological functioning. This can present as paralysis down one side of the body (hemiplegia), muscle weakness and imbalance, speech problems and changes in sensation.
Source: Stroke Association
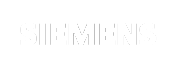
Image provided by HEIA-FR university
Wear and walk
Many stroke patients are already benefitting from robotic exoskeletons, which offer numerous benefits along the road to regaining mobility. They allow for more effective physiotherapy sessions, greater patient comfort, and can even provide quantitative information about the patient’s recovery such as velocity, smoothness and range of motion[4]. Various clinical studies have suggested that the use of exoskeletons in rehabilitation therapy can offer greater biomedical benefits than more traditional, passive orthoses such as braces and supports.
But while this burgeoning field of biotechnology is rapidly gathering pace, robotic exoskeleton design is still in its infancy, with many practical challenges like mass and size to overcome.
So, how are engineering teams around the world working to advance exoskeleton designs and take this life-changing technology forward?
Innovating the exoskeleton
When mechanical engineer Emmanuel Viennet was starting out in his career, medical science couldn’t have been further from his mind. He spent three years as a simulation engineer in the field of vehicle transmission systems, before coming to specialize in hydraulics. These days, he is a professor of mechanical engineering at Switzerland’s HEIA-FR university and, through his work in fluid power technology and system simulation, is helping advance stroke rehabilitation technologies like exoskeletons in novel ways.
“Our current project focuses on the development of a hydraulic actuator for an ankle exoskeleton that would be used by stroke patients in rehabilitation settings,” he explains. The project—named Talaris after the winged sandals of Hermes, the Greek messenger god— investigates harnessing fluid power technology, which uses the natural flow of pressurized fluid as an energy supply to a hydraulic system as a means of powering the lower-limb device. This represents a departure from common exoskeleton designs relying on electric motors which can be noisy, heavy and bulky for the wearer[5].
The design challenge for Viennet and his team was to build a demonstrator of the innovative hydraulic-powered concept—but within the limitations of the university department’s finite financial resources. The nature of the concept also posed tough questions around testing. Viennet says his team generated around a dozen viable a priori variants by combining different hydraulic architectures, distribution principles, actuator types and energy storage components. But with the means to only build and test a maximum of two solutions, how would his team choose between pump-controlled or valve-controlled distribution, or decide on the best kind cylinder type?
This was where Viennet’s background as a simulation engineer came into play and resulted in him introducing Siemens Simcenter to this ground-breaking project. Using Simcenter Amesim, a powerful software for modelling and analysis of multi-domain systems, the Talaris team was able to evaluate their potential designs with ease in numerical simulations and preliminary tests, then make decisions with confidence.
“Thanks to Simcenter Amesim, we could narrow down our initial design ideas and thoroughly investigate our two final design candidates.” Emmanuel Viennet, HEIA-FR University
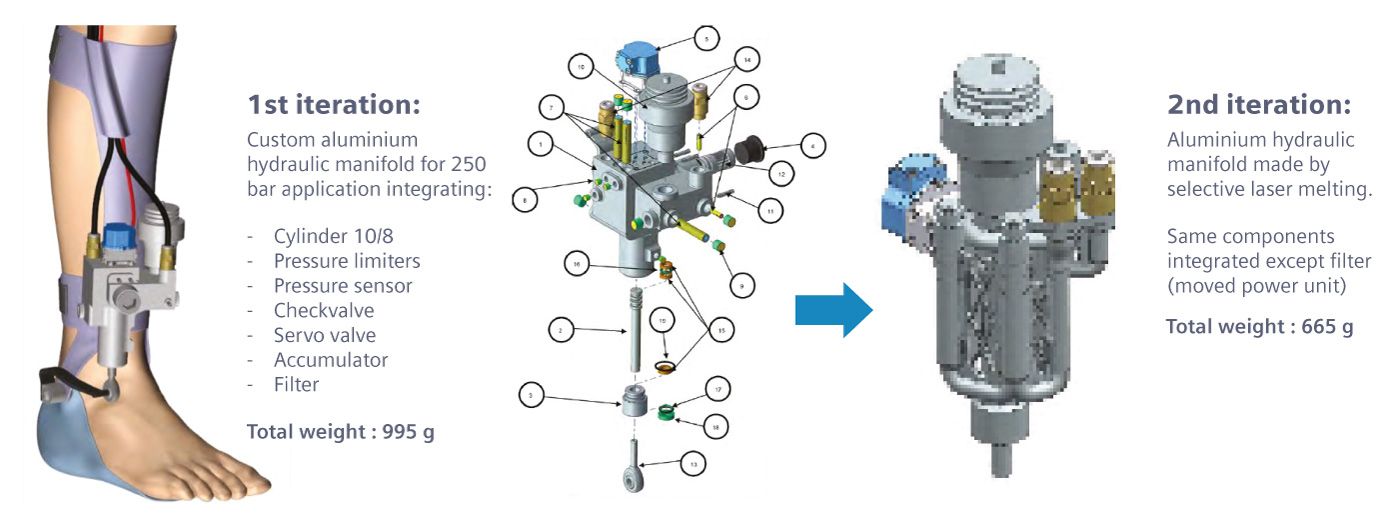
Image provided by HEIA-FR university. First concept for integration of the actuator on an exoskeleton stricture and design iterations
Testing the possibilities
The winning design featured a servo-hydraulic actuation rather than an electro-hydraulic solution, after Simcenter Amesim helped the team identify the option for best dynamic performance based on an ankle exoskeleton to support an 80kg patient when walking at a normal speed requiring the whole system to have a bandwidth of at least 8 hertz (Hz).
“Without simulation, we would have used more classical tools like spreadsheet, which would have limited ourselves to steady state analysis. On the other hand, we would have built more prototypes to reach the same level of system understanding,” Viennet says.
“Simcenter Amesim helps us by serving as a virtual test platform where design space can be narrowed down in a systematic and efficient way. In a less expected way, it also helps in providing a technology-neutral platform that can be leveraged by users to dive into domains they are unfamiliar with,” adds Viennet.
This opens the door to teams with diverse skillsets and domain expertise coming together to innovate, experiment and create. The low-risk environment simulation provides means that imaginations can be stretched to their fullest—and the potential outcomes are limitless.
In the world of stroke rehabilitation, exoskeletons are undoubtedly changing the game by harnessing technology and engineering excellence to help patients walk again while reducing the burden of lengthier recoveries for healthcare institutions. A recent review of exoskeleton technology[6] published in the Journal of Neuro-Engineering and Rehabilitation, however, saw the authors point out that wearable robotic exoskeletons—a relatively nascent approach to rehabilitation since their first use in 1994—still have some way to go in terms of optimal design. Based on a review of exoskeletons currently in use in rehabilitation setting, the report is a reminder that wearer comfort, complexity of fitting and operation and the device’s ability to mimic natural gait are areas of design that must be improved in the future. As Emmanuel Viennet’s work at HEIA-FR University illustrates, simulation has a central role to play in realizing those improvements.
References
- http://www.emro.who.int/health-topics/stroke-cerebrovascular-accident/index.html
- According to research by University of Applied Sciences and Arts in Western Switzerland
- https://www.ahajournals.org/doi/10.1161/STROKEAHA.120.029606
- https://www.sciencedirect.com/topics/engineering/exoskeleton-robotics
- https://www.researchgate.net/publication/336519948_Development_and_Control_of_an_Electro-Hydraulic_Actuator_System_for_an_Exoskeleton_Robot
- https://jneuroengrehab.biomedcentral.com/articles/10.1186/s12984-021-00815-5